
LED Heat Lamp Therapy Part 1: Energy Dosing
There is a new form of light therapy that has been recently invented in the past couple of years. It is called LED Heat Lamp Therapy, which uses high-intensity Red & NIR LED panels for therapeutic heating and photonic energy delivery.
These are no longer true Red Light Therapy as that follows the non-thermal light therapy sciences of Low Level Light Therapy and Photobiomodulation. As we discuss in great detail in a previous blog.
As is the basic definition described in most studies:
"Instead of utilizing heat, PBM harnesses the photochemical conversion potential of low-intensity near-infrared (FR/NIR) light within the range of 630–1000 nm.15–18"
[1]
The quote above, like many others we find, emphasizes that heat is not utilized for PBM.
With the essential detail of being low intensity that does not cause significant heating as Dr. Hamblin describes in this article below:
"The reason why the technique is termed LOW-level is that the optimum levels of energy density delivered are low when compared to other forms of laser therapy as practiced for ablation, cutting, and thermally coagulating tissue. In general, the power densities used for LLLT are lower than those needed to produce heating of tissue, i.e., less than 100 mW/cm2, depending on wavelength and tissue type."
[2]
The optimum intensities for LLLT and PBM must fit the criteria to be low enough to not cause heating. For a small laser beam this is usually <100mW/cm^2, for large treatment area devices we find this is generally <50mW/cm^2.
We are at a pivotal moment in light therapy history with this discovery. LLLT was also accidentally discovered by Endre Mester in the 1960's when he used a low power laser on rats. He had meant to use a higher-powered laser, but was surprised at the result that the low power laser caused a biostimulatory responses like improved hair growth and wound healing.
Now in 2024, many brands have accidentally discovered LED Heat Lamp Therapy by making unprecedentedly high powered panels, measuring them with solar power meters, hiring influencers to promote them, and then experimenting on humans with them without informed consent.
Thus, we find many devices are now in an entirely new category of of light therapy, since high-intensity LED panels will cause significant heating on the skin and will no longer be categorized as LLLT or PBM. These blogs will be the first to document and explore the scientific concepts for LED Heat Lamp Therapy.
*Medical Disclaimer* This blog is for educational purposes and is not to be used as medical advice. We recommend consulting with a doctor before proceeding with any therapies or treatments, especially experimental ones like high intensity light therapy that haven't been fully studied.
Summary: How to use LED Heat Lamp Therapy
You could use standard LLLT/PBM dosing (2-10 J/cm^2) and calculate your exposure time to be very limited with high-intensity panels. Our dosing calculator on another blog can help make sure high intensities are not being overdosed.
Since high-intensity devices promise to deliver significantly better penetration, then it is even more important to start with proper low doses 2-10 J/cm^2, even for deep tissue treatments. Where for true LLLT/PBM the higher doses up to 50 J/cm^2 are used for deeper tissue due to having less penetration.
Preferred wavelengths for High-Intensity light therapy are NIR larger than 800nm. This is important for the goal of deeper penetration, but to also avoid the superficial heating caused by Red light or shorter wavelengths that could cause burning or damage.
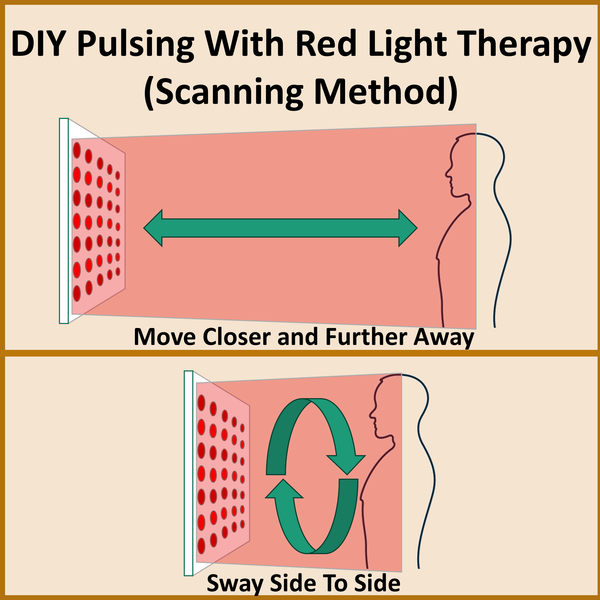
Pulsing and Scanning modes will also be more important for LED Heat Lamp Therapy to reduce the risk of overheating and burns, similar to high intensity Lasers.
Applications: The best known applications of high-intensity red light therapy are for temporary pain relief, muscle relaxation, wound healing, inflammation reduction, and various musculoskeletal pain conditions.
Safety: High intensity light therapy runs the risk of burns if using excessive temperatures for long periods of time or repetitively. Erthyma Ab Inge is a hyperpigmentation response that can occur from sustained or repeated heat therapy. Erthyma is the skin redness similar to sunburn. Blood pressure drops from Nitric Oxide release may be a precaution with people with hypotension (low blood pressure).
A New Light Therapy:
Large LED Arrays (panels) delivering high power density (>50mW/cm^2) will often deliver a heating effect on the tissue. Thus no longer meeting the basic definitions of Low Level Light Therapy (LLLT) or Photobiomodulation (PBM) which we cover in a previous blog is well-known as being a non-thermal "cold" light therapy.
These new high-intensity LED devices must be studied under a different therapeutic category: especially for proper dosing, safety, mechanisms, and benefits.
Studies have identified a new category called High-Intensity Laser Therapy (HILT), a separate therapy from LLLT or PBM. These HILT lasers use higher powers than typical LLLT cold lasers.
"Unlike LLLT, HILT produces a thermic effect on the treated tissues."
[4]
Again emphasizing the lack of thermic (heat) effect from true LLLT.
Since high-intensity LED Panels also produce a thermic (heat) effect, then a new category of therapy could be High Intensity Light Therapy (HILT) that also uses LEDs. Similar to how LEDs initially piggy-backed into LLLT. Or a more common term will be LED Heat Lamps, similar to how we refer to Incandescent NIR Heat Lamps.
In this blog, we will be examining the potential dosing in the Laser therapy called HILT, and implications on high-intensity LED devices, however it may be irrelevant due to natural differences in LED and Laser.
Heat And Light Therapy: Better Together?
We like to assume that Red Light Therapy and Heat are complimentary to do together.
However, as PBM and LLLT are typically a "cold" light therapy, it is usually optimized by using techniques that minimize heating like non-thermal wavelengths, low intensity, pulsing that allows tissue cooling between pulses, scanning methods, and external cooling like cold packs and cold air.
Heating has been documented to decrease the penetration of light by increasing blood vessel volume and blood flow.[4] Heat has been also attributed to a rise in ROS when combined with Red/NIR light, which would play a role in the inhibitory responses (biphasic dosing).[5]
Like combining any medicines or therapies - the best thing to do is to truly test your theories. Salespeople using rhetorical arguments that "sunlight is warm" and that the "heating feels good and anecdotally is beneficial" only confirms an apparent lack of science to back up this combination of Light and Heat therapies.
Studies on HILT are indeed very positive on their speculations that you get the best of both worlds when you combine light therapy and heating.
"low-level laser therapy (LLLT) and high-intensity laser therapy (HILT) while both shared similar photo-biomodulation and anti-inflammatory effects, LLLT (energy output ≤500 mW) reaches superficial tissues only, while HILT (energy output >500 mW) can reach deeper tissues. In addition, HILT can produce photothermal effects [7, 8]."
[6]
With the quote above emphasizing the difference that HILT adds the photothermal effects whereas LLLT does not have thermal effects.
One study states:
"HILT offers distinct advantages over LLLT as it enables the delivery of higher energy over time. HILT allows for more energy deposition in deep tissues, resulting in both the biological effects of LLLT and thermal effects [13, 14, 18]."
[7]
The contrast is important that if you are having thermal effects then you simply aren't doing LLLT/PBMT. Adding heat to PBM simply becomes a different type of therapy like HILT.
And another study states:
"HILT is hypothesized to have similar properties to LLLT, but with augmented effects due to its higher power. A commonly mentioned advantage of HILT is that, with increased power, the depth of penetration may also increase (ref)."
[8]
Although many studies mention HILT is implied to have better penetration than LLLT, I have not seen any comparative data to confirm. Ironically the quote above has a placeholder for a reference (ref), but the author likely forgot to add the citation.
One article notes that LLLT average penetration is 2-4 cm, and HILT average penetration is 10-20 cm. But they do emphasize the use of NIR for HILT for deeper penetration. [7]
Another article says:
"These advantages include (i) a higher energy output than low-level laser therapy [11]; (ii) an anti-inflammatory effect with pain modulation and impact on nerve endings for pain relief [8,11]; and (iii) a scattering mode of laser radiation with therapeutic photo-thermal effects that induce localized muscle relaxation, reducing muscle spasms [13]."
[10]
The researchers conducting HILT trials are assuming it combines the benefits of LLLT with heating as well as potentially better penetration due to the nature of high intensity. Some studies mention a Photomechanical and Photothermal effect only gotten by HILT, and not from LLLT which is only a Photochemical effect.
Dosing High Intensity Devices
Even if we can make hypothetical arguments that Light and Heat combined are beneficial, then we once again have made "red light therapy" much more complicated by adding a new variable of heat.
As always, the devil is in the details. How do you properly dose high intensity heating devices? How do you make sure it is safe? That it is effective and optimal?
In HILT, doses are ranging from typical PBM doses (2-10 J/cm^2) up to hundreds or even thousands of J/cm^2. [11] There aren't as solid dosing guidelines like we have for cold LLLT/PBM.
"One group preferred to use a fluence (energy density) range of 9 to 225 J/cm2 while another group reduced fluence to 1.2 to 6 J/ cm2."
[11]
Even if we had consistent HILT dosing, a small laser dose will be very different than a large high-powered LED panel.
HILT studies may not be relevant at this time for commercial LED panels until they actually start doing HILT studies with larger devices.
Low Intensity Light Therapy (LLLT) vs High Intensity Light Therapy (HILT)
In various musculoskeletal conditions and pain, there have been a few trials comparing LLLT and HILT.
One study found that HILT performed better than LLLT on 98 humans with carpel tunnel. Both used the same dose of 8 J/cm^2 or 20 J/cm^2 and found the High Intensity Laser Treatment was most effective at 8 J/cm^2. [11]
Confirming a biphasic dose response as the 20 J/cm^2 was not effective, even in a human study. The LLLT was 50mW and HILT was 1,600 mW, but the intensity was not specified (the size of the laser spot was not specified so I can't calculate it either). [11]
Both LLLT and HILT showed improvement, the HILT had better results overall. And even with HILT the biphasic dose response must be observed.
One study compared LLLT and HILT on plantar fasciitis in 102 humans and found that both groups improved, but no significant difference was found between HILT vs LLLT. The parameters of both lasers were very different, both treatments were around 7 minutes with a dose of 4 J/cm^2 for LLLT and a dose of 120 J/cm^2 for HILT. [12]
Another study used LLLT of 400mW and HILT of 5,000mW again with unspecified intensity. The LLLT was 830nm at 10 to 12 J/cm^2 and the HILT was 1064nm at 19 to 150 J/cm^2. Both groups saw improvement for Knee Osteoarthritis, but the HILT group saw statistically significantly more benefit. [13]
They acknowledge the differences in wavelengths and dose also could have an impact. They note the LLLT could be more effective used in the stationary mode (holding it still), and there is a preference to use HILT to be used in the scanning mode (slowly moving it back and fourth across the treatment area).
Another review article discusses comparisons of LLLT to HILT used for musculoskeletal and found a lack of consistency to determine which would be better. They suggest more studies on this topic.
"A well-designed RCT should be conducted to compare the effects of LLLT versus HILT for musculoskeletal pain disorders in order to confirm or infirm the superiority of HILT over LLLT."
[14]
Since LLLT did indeed provide benefits in all of these cases, we emphasize our point to start with the safest, low intensity, low dose treatments. In most cases this produces a beneficial healing response, and only carefully implement higher intensities as needed.
High Intensity - Pulsing and Scanning Modes Required
For safety and to manage the heating produced by high intensities, then pulsing and scanning techniques become almost essential for effective usage of HILT.
"Furthermore, it has been suggested that pulsed mode could yield better outcomes than continuous laser mode because the photothermal effects can be controlled and limited for patient safety by modulating pulse intensity and frequency"
[14]
Pulsing essentially allows for higher peak intensities while reducing the average intensity. During the "off" time of the pulses it gives the tissue a small amount of time to cool off and thermoregulate.
Another article comments on how scanning high intensity lasers (waving them slowly back and forth over the treatment area) is a more effective way to deliver HILT.
"Moreover, with specific consideration of HILT (as it delivers a higher dose of laser energy), scanning mode is preferable as it theoretically allows for deeper penetration, greater stimulation of cellular processes, and better heat dissemination (to avoid skin burn) [18]."
[10]
Implementation of High Intensities in LED Panels:
If high intensities were to be properly implemented into LED panels, it would require more complex electronics like pulsing modes to reduce the heat on the skin. As that is the primary reason studies use pulsing anyway is to allow the skin to cool between pulses, not for any magical mechanisms related to the pulse frequency itself.
It would require more from the consumer/patient/user to understand the scanning method and wave their device of body around to avoid the heat. Or perhaps use a cooling fan aimed at the patient to also reduce the heating on the skin.
LED Heat Lamps would need to use more of the ratio of wavelengths in the Near-Infrared to deliver on the promise of deeper penetration and avoid problematic heating caused by superficial Red wavelength absorption. For example the typical 50/50 split of Red/NIR would be inappropriate for high intensity LED panels, and should favor a much higher % in the NIR, or perhaps no Red at all.
In other words, simply standing in front of a low intensity true PBM panel for 10-20 minutes will become much more complicated with high intensities. We find many people are just now grasping the proper distance to use a panel, but now manufacturers will require them to dance around in circles as a type of scanning method.
Quick Doses with High Intensity
One study on 114 people with Plantar Fasciitis used either a 10W or 25W laser for a dose of 10 J/cm^2. Both groups got similar results in reduction of pain, showing that a dramatically higher intensity does not inherently get better results.
[15]
This is another example where seemingly "low" doses of 10 J/cm^2 are used for deep tissue, because the high intensity lasers penetrate deeper.
Heat Safety with LED Heat Lamps
Heat is an inevitable consequence of any energy therapy, although in LLLT and PBM it is managed and minimized as much as possible.
One study notes that monitoring tissue temperature will be important to understand the thermal effects of PBM. This will be important for Part 2 of this series.
"We demonstrate in this study that simply monitoring surface temperature is a very potent real-time clinical biomarker to ensure treatment safety."
"We strongly advocate reporting treatment surface irradiance and surface temperature, when available, in future PBM studies to aid in robust future reproducibility of specific treatment protocols."
[16]
One PBM article investigated the possible influence of heating on the therapy titled "Photothermal Effects of High-Energy Photobiomodulation Therapies: An In Vitro Investigation".
It notes that a small temperature increase of 1-2 C is potentially advantageous, but excessive or sustained temperature increase is detrimental. Even up to 6 C increase is acceptable as long as the temperature stays below 45C.
"It is accepted that beyond this extra 6 °C level, there is the potential for permanent deformation of structural tissue proteins to occur, as well as perhaps other biomolecules, when subjected to protracted exposure to temperatures above 45 °C"
[17]
Another PBM article reinforces this position of excessive temperatures from high intensities that could cause damage.
"But rising tissue temperature above 45° C causes irreversible damage [15]."
[18]
Luckily, the skin should detect significant heating at 41°C to pull away, and heat pain should be triggered at 43-45°C. However, this also means that high intensity light therapies are contraindicated for people that might not have normal heat sensations.
Regardless, the most prudent advice for safely using high intensity devices would be to monitor skin temperature for the safe temperature range, especially since skin tone, skin thickness, and circulation will all affect individual's heating response. We cannot use intensity alone to understand the expected amount of heating.
Heat in the PBM Therapy? Or PBM in the Heat Therapy?
One 2022 PBM study used a 780nm LED at 3,800 mW/cm^2 for 3 minutes (pulsed) to treat neck and shoulder pain in humans. The dose was reported as 570 J/cm^2. [19]
They monitored skin temperature was risen on average of 6.8C up to about 41C. [19]
Skin redness was observed in 9 out of 10 patients due to the heating. This will likely be a common side effect for high-intensity Red Light Therapies in the future, although it is rarely reported since most PBM studies avoid causing significant heating like this. As well we already know one study found these side effects at 480 J/cm^2.
It is important to note that high intensities and/or doses of Red Light Therapy do well for temporary pain relief by leveraging the inhibitory side of the biphasic dose response. Specifically inhibiting the pain signals by nerve cells. This we show in our dosing blog as the analgesia region of the dosing graph. So for temporary pain relief high intensities and doses may be prefered, at the detriment of slower healing.
Which may explain the preference for HILT to be used in mostly areas of musculoscheletal pain management.
As the authors correctly point out, they cannot discern if the benefits were entirely from the PBM effects, the heat, or the combination. Especially since both PBM and Heat Therapy could certainly be used to treat areas of pain.
"One possible mechanism for the effectiveness of our device may be the physiological changes caused by the increase in skin temperature."
[19]
In most other PBM/LLLT studies they are clear that the benefits and gotten are from non-thermal interactions and mechanisms. The reason why heating is separated from PBM is illustrated by this study, that heat therapy mechanisms could end up influencing or dominating the effects.
Practical High Intensity Light Therapy
More information on the differences between LLLT and HILT can be found in the article below.
It contains many practical tips for the application of HILT like pulsing, longer wavelengths, and that HILT is almost always non-contact to prevent overheating of the skin.
A fun fact according to the article; While we know LLLT was discovered in the 1960's and had it's first FDA approval for treating pain in 2001 - HILT was first published in 2009.
This is why LLLT/PBM has such a larger pool of studies and benefits. The article shows the contrast that LLLT has many more clinically studied treatments than HILT at this point.
Conclusion - HILT is Not LED Panels:
It is important to remember the major differences between High Intensity Lasers and high intensity LEDs.
We can find a parallel that high-intensity LED Heat Lamps cause heat similar to HILT. LED Heat Lamps cannot fit in the PBM or LLLT categories due to heating.
In terms of the promise of higher penetration with high intensities, the (peak) intensities used in HILT are on the scale of thousands of mW/cm^2. [16]
So a "high intensity" LED panel only emitting 50-500 mW/cm^2 are still nowhere near the intensities needed for the penetration promised by HILT delivered by lasers. Despite many salespeople promising that their overpowered non-contact LED panels magically deliver deep penetration.
Truly high-intensity LED Panels would need similar modes as HILT like pulsing and scanning to properly manage the heat. Perhaps even abandoning Red wavelengths entirely and only using NIR to reduce heating and focus on deeper penetration.
We can see even for HILT that proper Energy Density (J/cm^2) will be even more important.
Since high intensities supposedly deliver deeper penetration, then proper dosages are often less than or equal to 10 J/cm^2. For LLLT sometimes the dosage is higher 10-50 J/cm^2 for deeper tissue, but since HILT penetrates deeper by virtue of high intensity, then the dosage usually needs to be lower.
High Intensity Laser Therapy appears to be chosen for various areas of musculoskeletal issues and pain. It is a new area of research compared to LLLT/PBM so proper dosing and applications have not been fully studied.
There is clearly a lot of hype and competition for LED Panels to deliver high intensity based on speculative superiority of benefits and penetration. Often encouraged by fake experts that don't understand the basic definition of LLLT/PBM as being non-thermal. This has easily crossed the line into an entirely new category of therapy that has not yet been studied.
High-Intensity LED Heat Lamps could indeed be implemented for the benefit of humanity, but only when it receives proper scientific research and it is mindfully implemented. In part 2 we will explore using them as a true heat therapy.
Until then, the promise of speculative benefits and lack of dosing guidance don't outweigh the massive amount of safety and effectiveness already proven by non-thermal LLLT/PBM.
References:
[1]
Siqueira RC. Photobiomodulation Using Light-Emitting Diode (LED) for Treatment of Retinal Diseases. Clin Ophthalmol. 2024;18:215-225. Published 2024 Jan 22. doi:10.2147/OPTH.S441962
[2]
Hamblin, MR. MECHANISMS OF LOW LEVEL LIGHT THERAPY
http://photobiology.info/Hamblin.html
[3]
Chaki C, De Taboada L, Tse KM. Three-dimensional irradiance and temperature distributions resulting from transdermal application of laser light to human knee-A numerical approach. J Biophotonics. 2023 Sep;16(9):e202200283. doi: 10.1002/jbio.202200283. Epub 2023 Jun 14. PMID: 37261434.
https://pubmed.ncbi.nlm.nih.gov/37261434/
[4]
Tanaka Y, Tsunemi Y, Kawashima M, Tatewaki N, Nishida H. Objective assessment of skin tightening in Asians using a water-filtered near-infrared (1,000-1,800 nm) device with contact-cooling and freezer-stored gel. Clin Cosmet Investig Dermatol. 2013;6:167-176. Published 2013 Jun 26. doi:10.2147/CCID.S47299
[5]
The effects of infrared radiation on the human skin
Luke Horton, Joshua Brady, Colin M. Kincaid, Angeli Eloise Torres, Henry W. Lim
First published: 11 July 2023
https://doi.org/10.1111/phpp.12899
https://onlinelibrary.wiley.com/doi/10.1111/phpp.12899
[6]
Xie YH, Liao MX, Lam FMH, Gu YM, Hewith A Fernando WC, Liao LR, Pang MYC. The effectiveness of high-intensity laser therapy in individuals with neck pain: a systematic review and meta-analysis. Physiotherapy. 2023 Jul 20;121:23-36. doi: 10.1016/j.physio.2023.07.003. Epub ahead of print. PMID: 37812850.
https://www.physiotherapyjournal.com/article/S0031-9406(23)00037-8/fulltext
[7]
de la Barra Ortiz, H.A., Avila, M.A., Miranda, L.G. et al. Effect of high-intensity laser therapy in patients with non-specific chronic neck pain: study protocol for a randomized controlled trial. Trials 24, 563 (2023). https://doi.org/10.1186/s13063-023-07599-0
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10472636/
[8]
Starzec-Proserpio M, Grigol Bardin M, Fradette J, et al. High-Intensity Laser Therapy (HILT) as an Emerging Treatment for Vulvodynia and Chronic Musculoskeletal Pain Disorders: A Systematic Review of Treatment Efficacy. J Clin Med. 2022;11(13):3701. Published 2022 Jun 27. doi:10.3390/jcm11133701
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9267539/
[9]
de la Barra Ortiz HA, Avila MA, Miranda LG, Liebano RE. Effect of high-intensity laser therapy in patients with non-specific chronic neck pain: study protocol for a randomized controlled trial. Trials. 2023;24(1):563. Published 2023 Aug 31. doi:10.1186/s13063-023-07599-0
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10472636/
[10]
Ahmad MA, Moganan M, A Hamid MS, Sulaiman N, Moorthy U, Hasnan N, Yusof A. Comparison between Low-Level and High-Intensity Laser Therapy as an Adjunctive Treatment for Knee Osteoarthritis: A Randomized, Double-Blind Clinical Trial. Life. 2023; 13(7):1519. https://doi.org/10.3390/life13071519
https://www.mdpi.com/2075-1729/13/7/1519
[11]
Ezzati K, Laakso EL, Saberi A, Yousefzadeh Chabok S, Nasiri E, Bakhshayesh Eghbali B. A comparative study of the dose-dependent effects of low level and high intensity photobiomodulation (laser) therapy on pain and electrophysiological parameters in patients with carpal tunnel syndrome. Eur J Phys Rehabil Med. 2020 Dec;56(6):733-740. doi: 10.23736/S1973-9087.19.05835-0. Epub 2019 Nov 18. PMID: 31742366.
https://pubmed.ncbi.nlm.nih.gov/31742366/
[12]
Naruseviciute D, Kubilius R. The effect of high-intensity versus low-level laser therapy in the management of plantar fasciitis: randomized participant blind controlled trial. Clinical Rehabilitation. 2020;34(8):1072-1082. doi:10.1177/0269215520929073
https://journals.sagepub.com/doi/10.1177/0269215520929073
[13]
Ahmad MA, Moganan M, A Hamid MS, Sulaiman N, Moorthy U, Hasnan N, Yusof A. Comparison between Low-Level and High-Intensity Laser Therapy as an Adjunctive Treatment for Knee Osteoarthritis: A Randomized, Double-Blind Clinical Trial. Life (Basel). 2023 Jul 6;13(7):1519. doi: 10.3390/life13071519. PMID: 37511894; PMCID: PMC10381799.
https://pubmed.ncbi.nlm.nih.gov/37511894/
[14]
Starzec-Proserpio M, Grigol Bardin M, Fradette J, et al. High-Intensity Laser Therapy (HILT) as an Emerging Treatment for Vulvodynia and Chronic Musculoskeletal Pain Disorders: A Systematic Review of Treatment Efficacy. J Clin Med. 2022;11(13):3701. Published 2022 Jun 27. doi:10.3390/jcm11133701
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9267539/
[15]
Ketz AK, Anders J, Orina J, et al. Photobiomodulation Therapy Plus Usual Care Is Better than Usual Care Alone for Plantar Fasciitis: A Randomized Controlled Trial. Int J Sports Phys Ther. 2024;19(1):1438-1453. Published 2024 Jan 2. doi:10.26603/001c.90589
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10761604/
[16]
KHAN, I., ARANY, P.. Dosimetry for photobiomodulation therapy: response to Sommers et al. Annals of Translational Medicine, North America, 4, may. 2016. Available at: <https://atm.amegroups.org/article/view/10516>. Date accessed: 01 Mar. 2024.
https://atm.amegroups.org/article/view/10516/11143
[17]
Cronshaw M, Parker S, Grootveld M, Lynch E. Photothermal Effects of High-Energy Photobiomodulation Therapies: An In Vitro Investigation. Biomedicines. 2023;11(6):1634. Published 2023 Jun 4. doi:10.3390/biomedicines11061634
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10295700/
[18]
Durmuş, Hüseyin & Gün, Neslişah & Karaböce, Baki & Seyidov, Mirhasan. (2021). Investigation of temperature effects of a low-level laser source within the muscle phantom. International Journal of Advances in Applied Sciences. 10. 373. 10.11591/ijaas.v10.i4.pp373-377.
[19]
Odagiri K, Yamauchi K, Toda M, et al. Feasibility study of a LED light irradiation device for the treatment of chronic neck with shoulder muscle pain/stiffness. PLoS One. 2022;17(10):e0276320. Published 2022 Oct 17. doi:10.1371/journal.pone.0276320